Joy in Medicine Program
Joy In Medicine: How To Track Progress
The Joy in Medicine Recognition Health System Program is increasingly popular.
Is there an easy way to track your progress?
The Joy in Medicine program is designed to improve physician satisfaction and reduce burnout.
The goal is to spark positive change. To guide health care organizations towards a culture where you increase and maintain wellbeing among your staff.
The American Medical Association launched the initiative in 2019.
Fast forward and research shows that today burnout and stress levels are record high.
COVID has undoubtedly had a negative impact on physicians’ wellbeing.
The Joy in Medicine Recognition Program
When clinicians start their profession, their passion burns bright.
Few would like to imagine themselves as burnout, possibly just within a few years.
But research shows the reality is harsh.
Anxiety, depression, stress, work overload, and burnout are real.
How can we turn the tide?
This is how the AMA program helps health care professionals:
1. Roadmap to carry out ideas, programs, and policies to improve wellbeing
2. Help build a caring culture that unites everyone in the organization
3. Create awareness about tools and solutions to spark joy in medicine and the importance of investing in these to something about physician burnout
This is about moving your people to take action!
As you start to improve patient care, increase efficiencies, and bring up staff satisfaction, joy will spread.
“The Joy in Medicine Recognition Program is designed by the AMA to serve as a guide and catalyst for organizations who are interested, engaged and committed in efforts to fight the root causes of physician burnout,” said AMA Board Chair Jesse M. Ehrenfeld, M.D., M.P.H.
How and where do you start to promote joy?
Burnout is not an individual problem, it’s a systemic issue in the profession.
It doesn’t only have devastating effects for your healthcare workers, it also hinders great care, affecting your patients.
So as you try to improve conditions for your workers, how do you know you’re on the right track?
There are 1000 things that you can do to promote a healthier workforce, you obviously have to choose to start with something.
Which hands-on action will you start with?
Now, the strategies that your implement and the actions your physician leaders take, are they pushing your culture in the right direction?
Are they having the desired effect on your physicians’ mental health and wellbeing?
How can you easily collect data to stay on course towards a better workplace and more joy in medicine?
Here’s a simple approach to continuous workplace improvement:
A fit-bit for employee wellbeing
At Celpax we like to see ourselves like a heart rate monitor you use for your daily runs.
A heart rate monitor is not a medical checkup (like the yearly survey), but all athletes use one to improve. It tracks how your training went, if you’re getting fit… our devices do the same, but for employee morale.
Our mood device hangs at the exit point of the hospital ward.
As your healthcare staff finishes their shifts, they take a moment to self-reflect on their workday.
They then choose to press a green or red smiley to answer “How was your day?”.
After hitting the feedback button, they are shown how the rest of the team felt their day went.
Using baseline methodologies, the question is a constant.
This Mood KPI shows you a stable baseline of how your people experience their workdays.
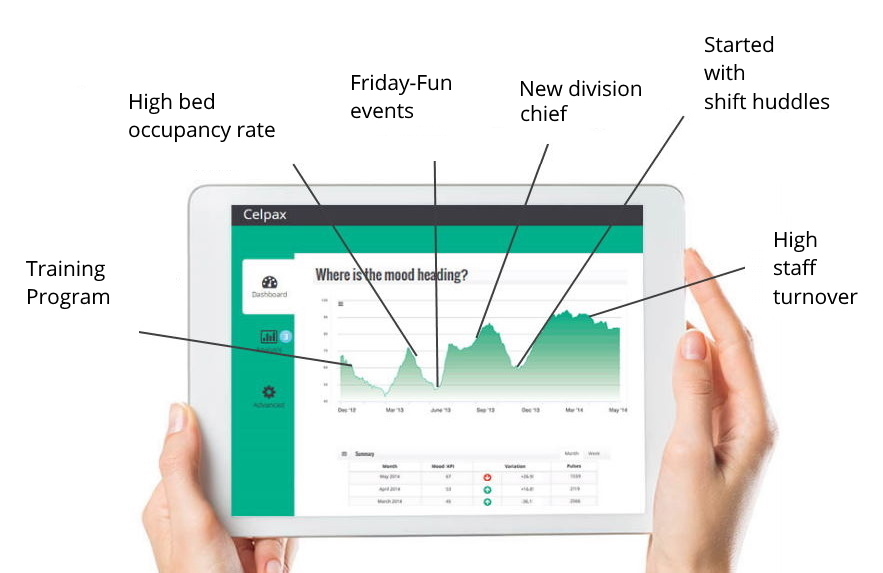
So if you get an average of 70% of people pressing green last month, what can you do to get a higher % of green this month?
And what happens on shifts when people press 90% green?
Or 25% green..?
With employee engagement surveys you get a lot of in-depth explanations. With the Celpax terminal, you get daily data while you improve, to stay on track.
- The old way of dealing with nurse burnout
Change something, then consult the data
Some of the problems at hospitals and clinics are chronic. Others are acute illnesses.
Both need to be carefully addressed.
But there is seldom a clear road ahead, and again, you have to choose what action comes next.
With the daily data, it’s easier to navigate as your healthcare leaders experiment and change. You’ll get instant employee morale data.
After talking with your team you change something, then consult the data.
Do your nurses feel they need a quiet space?
”In particular if there was a death on the unit or something else happened, they just needed a short break.”, says Chip Davis, President of Johns Hopkins Sibley Memorial Hospital.
Did employee morale get a boost out of bringing in therapy dogs to their medical intensive care unit?
If the data shows a lot of green, then you apply another change. And so on.
The method most of our healthcare providers use is to Measure, Talk, Improve. Repeat!

Early warning system
The daily data will give you an early warning if something bad is heading your way.
Perhaps there’s been a lot of staff changes lately.
Or unaddressed rumors of layoffs are taking a toll. Or a new unpopular schedule was pushed down from upper management.
Make sure your health care leaders take the time to regularly actively listen to what your employees say and do something about it.
Daily stand-ups, or shift meetings, is a great moment to quickly address whatever is cooking.
You can predict when a crisis is coming, and verify when you’re out of the crisis.
“It’s impressive how we came back. The motivation went up after staff meetings and just talking to people. I could see it in the Mood KPI numbers when we reached the bottom“, says user Dirk Feldhaus.
The preventive angle is also one of the reasons why insurance companies recommend the Celpax device to their clients, to reduce long-term exhaustion and diminished interest and get more productive employees.
- Reading tips: Joy in Medicine? What 100 Healthcare Professionals Have to Say about Job Satisfaction, Dissatisfaction, Burnout, and Joy, by Eve Shapiro.
It’s normal to have big differences
We’ve seen healthcare units with an average of 17% green feedback, and others with 90% green like the GI Clinic at Baylor Scott & White Health.
The data also tend to show differences between those working the “grave-yard” shift, and the day shifts.
And needless to say, pulling 15-hour shifts simply doesn’t tend to generate a lot of green feedback.
At first sight, it might seem like a no-brainer that a hospital ward where 9 out of 10 feel they had a GOOD day at work is better than one with 7 out of 10.
And yeah, it kind of is.
But.
This is also an instrument where the trend is many times more interesting than the number itself.
This is not a tool to get a nice employee engagement number to show off to upper management.
This is a tool for healthcare leaders that are DOERS.
Because maybe the ward where 7 out of 10 press green are trying out some new routines, policies, or projects.
And while you as a leader experiment with new things to improve, it’s NORMAL for stuff to go wrong.
Or for staff to feel that there’s a bit too much chaos right now. Sometimes things have to get worse before they get better.
Change takes time. Both for employees and for team leaders.
(And hey, sometimes it takes even longer for top management hehe.)
That is why the next part is so important for healthcare leaders at all levels:

Keep the conversation going
Fact:
Our data shows that units where leaders regularly hold open conversations have higher Mood KPIs.
This needs to happen at all levels to truly see a global effect, both department chairs, division chiefs, nurse managers, directors, staff nurses, and lower levels of hospital management.
A great workplace is everyone’s job.
What would happen to staff wellbeing if more physician leaders started practicing to show more empathy and kindness at work?
And regularly sit down with their teams to talk about how they’re doing lately at work?
It can be during the first 4 minutes of the daily shift meeting. Or take 15 minutes at the weekly meeting.
Or just check in with the first employee you bump into in the corridor.
What makes us press green here? What can we do to do get more green?
Many times, just hearing people out has a big effect.
It might not be “all they want”, but it’s a great start, and can have a tremendous impact on someone’s workday.
A safe environment
It’s also a great moment to introduce coping mechanisms to better handle workplace stress and a high workload.
“How can I learn from this? Is there something I did wrong? How can I do better? Is it something that the system is failing on? How can I make the system better?”
The opposite:
“How could I be so stupid? I’m probably not good enough. I harmed my patient. It’s all my fault,” — that approach doesn’t really lead to improvement and puts you at higher risk for additional medical errors and for burnout, says Bryan Bohman, MD.
Encourage your people to speak up, and make sure you create an environment where it’s absolutely safe to do so.
This will guide you towards high-functioning care practices.
- More ideas here to increase Joy in Medicine
- Tips for Measuring Joy in Work from the Institute for Healthcare Improvement.
How to track the progress of your Joy in Medicine Program
1. Impact on the day you announce
As you know how your healthcare teams feel on a “normal” workday, you can verify the impact the day you announce that you’re joining the Joy in Medicine Program.
If you normally get 60% green, will people react positively and the data will show a spike of 80% green?
2. Impact day you launch
The percentage of green you get on the day you kick-off and launch the initiative is an important indicator.
Are your people with you? Or do you need to go back and clarify and communicate further?
3. Impact of first initiatives
Check the impact as your first actions take place. What’s the impact on the day of the first training session?
Or the redesign of your physical space to reduce noise? A lunch roulette among the physicians? Or testing 5-minute mindfulness breaks?
4. The first month compared to the month before
Has there been an increase in green feedback, compared to the previous month?
5. Activities with the most impact during the first month/quarter
The Day Analysis section is where an easy star system grades your days. Which were the days with the highest mood last month or quarter?
What happened on those days? Was it the same for all wards, units, shifts, etc?
6. First quarter compared to last
Adjust and move forward. What new things can you experiment with? What do people want to happen next?
Give them the tools and resources needed. Help them knock the barriers preventing them from giving great patient care, and looking after themselves and their colleagues.
7. Crosscheck with burnout, staff retention, long-term sickness
You can use a simple Excel sheet to download all the mood data, and then crosscheck with other KPIs your healthcare organizations are monitoring.
What happens when you are understaffed, vs. when you’re not? What makes a work shift green at your hospital?
What happens on a shift when there is a lot of red? Has this changed over time?
Frontline managers are key when it comes to supporting caregivers in a caring and supportive way.
The 2022 Joy In Medicine Program application starts in January 2022.
Are you ready to empower your people and form more human connections?


 Hej! I’m Rebecca, cofounder at Celpax. We manufacture simple tech tools to improve workplaces. And build a better society while at it. Let’s talk about more ideas for Joy in Medicine?
Hej! I’m Rebecca, cofounder at Celpax. We manufacture simple tech tools to improve workplaces. And build a better society while at it. Let’s talk about more ideas for Joy in Medicine?
Similar interests
- Non Gamstop Casinos UK
- Slot Sites UK
- New Betting Sites UK
- Casinos Not On Gamstop
- Gambling Sites Not On Gamstop
- Casino Non Aams Sicuri
- UK Online Casinos Not On Gamstop
- Gambling Sites Not On Gamstop
- Sites Not On Gamstop
- Sites Not On Gamstop
- Non Gamstop Casino Sites UK
- Best Online Casino Canada
- UK Casino Not On Gamstop
- Non Gamstop Casinos
- Casinos Not On Gamstop
- Siti Scommesse
- Top Casino Sites UK
- Slots Not On Gamstop
- Casino En Ligne Meilleur Site
- Casinos Not On Gamstop
- Betting Sites UK
- Slots Not On Gamstop
- UK Casino Not On Gamstop
- Migliori Casino Online Non Aams
- Non Gamstop Casino UK
- Lista Casino Online Non Aams
- Meilleur Casino En Ligne
- Best Crypto Casino
- Casino En Ligne
- Casino Online
- Casino En Ligne France
- Paris Sportif Ufc
- Casino Jeux En Ligne
- Meilleur Casino En Ligne
- Bonus Free Spin Senza Deposito
- Casinò Non Aams Con Free Spin Senza Deposito
- Nuovi Casino Non Aams
- Migliori Casino Online
- Crypto Casino
- Casino Non Aams