The old way of dealing with nurse burnout
Today we’re talking nurse burnout:
COVID Nurse Burnout
Etti Rosenberg is a nurse and head of the policy and planning department at Clalit Health, the largest health organization in Israel.
They currently employ 13,000 nurses in 14 hospitals and 2500 community clinics.
Here are Etti’s words related to nurse burnout, as the vaccine effect is spreading in Isreal: meaning nurses and health care workers can finally start seeking closure.
But hang on.
We’re not talking about putting up your feet after a long nursing shift and waking up relaxed the next day.
“To be a nurse, you really have to care about people.” Whitney Neville said.
“But when an ICU is packed with COVID-19 patients, most of whom are likely to die, to protect yourself, you just shut down. You get to the point when you realize that you’ve become a machine. There’s only so many bags you can zip.”
We’re talking about nurses spending a full year with heightened stress levels, anxiety and real risk of nurse burnout.
Post-traumatic stress, anyone?
Nurse burnout due to COVID is real
How has your workload been the last year?
How many hours and extra shifts have you pulled?
Emotional exhaustion is spreading, a common burnout symptom.
93% of healthcare workers in the US are experiencing stress according to research.
A whopping 76% report exhaustion and burnout, as nurse-to-patient ratios tripled with staff shortage.
Many report a lack of support and recognition from their organization and managers.
Many nurses are battling their third wave of Covid-19.
Other health care workers are finally seeing some light at the end of the tunnel:
What prevents nurse burnout?
How can we avoid nurse burnout?
And make sure the emotional support is there from the organizations?
What helps us nurses deal with death, illness and suffering on a daily basis?
Probably a set of things that are right for workers in therapeutic professions who finds relief both at home and at work.
But when the Covid-19 epidemic started the way the nurses operated changed. And the regular methods no longer worked.
When the pandemic began, it was no longer about the patient and his or her family struggles.
In every household, there was fear, anxiety, uncertainty and concerns over older parents, so the methods for daily relief at work broke.
There was no entertainment and no private time to relax, reflect or vent.
At work during the epidemic patients were unexpectedly getting worse.
And the number of deceased who died in loneliness with no family around adds to the emotional burden.
What was left were ceremonies and togetherness.
Nurses tend to hug a lot, encourage each other, celebrate and mark events and holidays together. And we kept doing this even when we were afraid of passing the virus.
“We were doing everything we could, but the patients were not getting better,” says Karia Jackson, a 39-year-old nurse interviewed by Newsday.com.
“I would sit in my car in the driveway and I would just cry for maybe an hour. Nobody is really going to understand until they saw what you saw.”
How did nurses cope with COVID-19?
One way to avoid burnout was through writing Covid diaries on social media.
Please join me How Nurses coped withCOVID-19? One way was through writing covid diaries in Social Media As an Admin of a Facebook group I will portray today in my lecture at Ben Gurion University conference what was happening in every wave https://t.co/xKsrQBuhYw pic.twitter.com/ShORsptj70 — Etti Rosenberg (@etirose) March 22, 2021
She is a nurse manager and a therapist with animals Our own Michal Lowenstein came with her dog Jenny to comfort the nurses from Covid-19 ward . They were amazed by the way Jenny was a great help during theses times. At our Belinson hospital by @ClalitHealth #nursingtogether pic.twitter.com/6WdejVvHKB — Etti Rosenberg (@etirose) February 27, 2021
Nurses lean on each other
“The most notable impact is the mental health surge that we are seeing as a result of the steady stream of caring for very sick patients, experiencing higher than “typical” death rates, and having to work in conditions/situations that have not always provided consistent PPE, staffing or resources”, says doctor Bonnie Clipper.
This year brought a different understanding of life and our ability to control our plans.
Are we going to act differently when it’s over?
Nurse leaders lead by example.
It doesn’t matter how many years of experience they have, we work together and mentor each other.
Passion, persistence, and discipline were always the characteristics of nursing.
Don’t be afraid to sit at the table where decisions are being made.
With 70% of the health workforce being women (80% of which are nurses and midwives), only 25% are in leadership roles. Nurses and midwives need more than just recognition, but action.
We nurses, we lean on each other.
We talk a lot and listen to one another.
And even in the midst of the pandemic, we knew how to do this.
We are all still currently digesting the year of the Corona pandemic and the many consequences it brought.
Yet, we cling to the regular practices of nurses; To touch, hug, friendly conversations and listening are the ones that quadruple the nursing staff’s ability to recharge.
Even a pandemic will not change this.
Etti Rosenberg is a nurse and head of the policy and planning department at Clalit Health, the largest health organization in Israel.
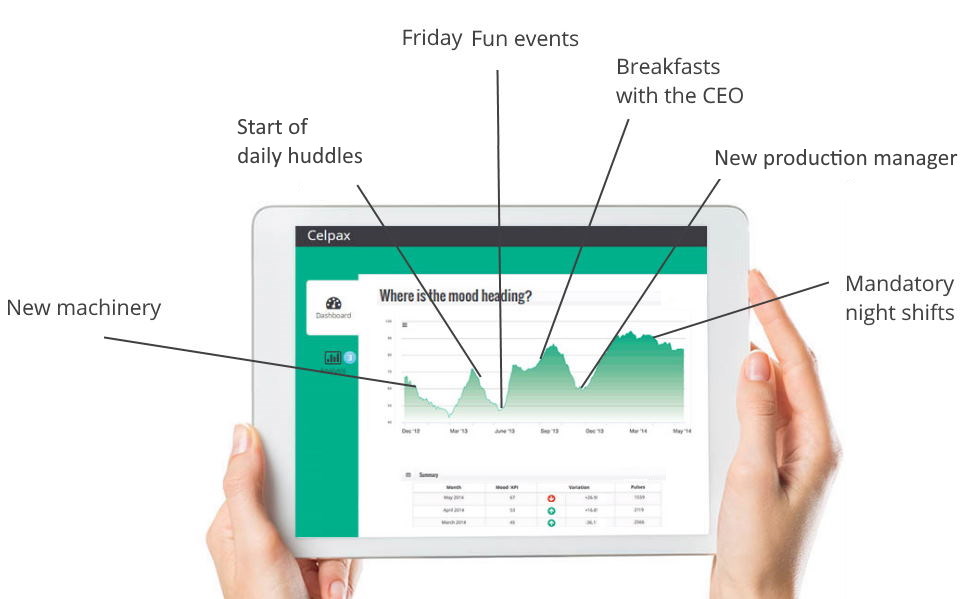
Measure if your leadership actions are working!
Get a survey kiosk.

Similar interests
- Non Gamstop Casinos UK
- Slot Sites UK
- New Betting Sites UK
- Casinos Not On Gamstop
- Gambling Sites Not On Gamstop
- Casino Non Aams Sicuri
- UK Online Casinos Not On Gamstop
- Gambling Sites Not On Gamstop
- Sites Not On Gamstop
- Sites Not On Gamstop
- Non Gamstop Casino Sites UK
- Best Online Casino Canada
- UK Casino Not On Gamstop
- Non Gamstop Casinos
- Casinos Not On Gamstop
- Siti Scommesse
- Top Casino Sites UK
- Slots Not On Gamstop
- Casino En Ligne Meilleur Site
- Casinos Not On Gamstop
- Betting Sites UK
- Slots Not On Gamstop
- UK Casino Not On Gamstop
- Migliori Casino Online Non Aams
- Non Gamstop Casino UK
- Lista Casino Online Non Aams
- Meilleur Casino En Ligne
- Best Crypto Casino
- Casino En Ligne
- Casino Online
- Casino En Ligne France
- Paris Sportif Ufc
- Casino Jeux En Ligne
- Meilleur Casino En Ligne
- Bonus Free Spin Senza Deposito
- Casinò Non Aams Con Free Spin Senza Deposito
- Nuovi Casino Non Aams
- Migliori Casino Online
- Crypto Casino
- Casino Non Aams